Airway and Alveolar Anatomy
Describe the function and structure of the upper, lower airway and alveolus.
Upper Airway
The upper airway consists of the:
- Mouth
- Nasal cavity
- Hairs filter large particles
- Olfactory receptors detect harmful gases prior to inhalation
- Pharynx
- Larynx
Breathing can be oral or nasal. Nasal breathing offers:
- Good humidification and filtration of inhaled particles because the septum and turbinates have:
- High mucosal surface area
- High mucosal blood flow
- Generate turbulent flow
- High resistance to flow
At a high minute ventilation, oral breathing is favoured.
Structures
- Pharyngeal dilator muscles
Including genioglossus and levator palati. Prevent pharyngeal collapse during negative-pressure ventilation and during sleep.
- Larynx
Important for airway protection, speech, and effort closure.- Prevents aspiration during swallowing by elevating the epiglottis and occluding of the aryepiglottic folds
- Phonation is achieved by adjusting tension (and therefore resonance) of the vocal cords by action of the cricothyroid
- During inspiration, cricoarytenoid muscles rotate the arytenoid cartilage and abduct the vocal cords to reduce resistance to airflow
- During expiration, the thyroarytenoid muscles adduct the cords and increase resistance, providing intrinsic PEEP
- Effort closure is tighter occlusion of the laryngeal inlet, in which the aryepiglottic muscles contract strongly to act as a sphincter, allowing the airway to withstand up to 120cmH2O of pressure.
Lower Airway
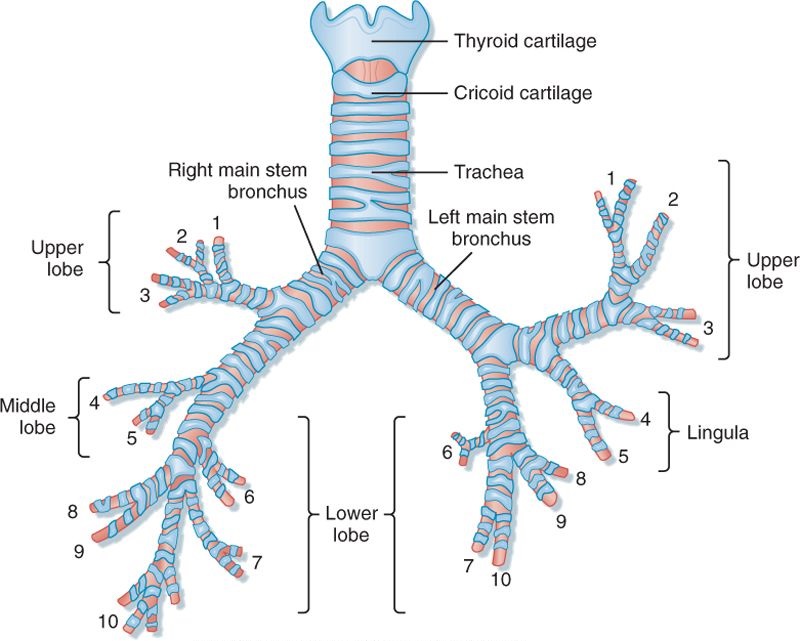
The lower airway consists of the tracheobronchial tree:
- From trachea to alveolus, the airways of the lungs divide 23 times
The tracheobronchial tree is divided into two zones, based on whether they contain alveoli and therefore are able to participate in gas exchange:- The conducting zone is the first 16 divisions
- The respiratory zone is the last 7 divisions
Conducting Zone
The first 16 divisions constitute the conducting zone:
- Anatomically, the conducting zone consists of:
- Trachea
- Mean diameter of 1.8 cm and a length of 11cm
- D-shaped cross section
Curved cartilages anteriorly and longitudinal muscle (trachealis) posteriorly. External pressure of 40cmH2O is sufficient to occlude the extrathoracic trachea. - Flow is typically turbulent in the trachea and large airways
- Bronchi
- Comprise the first four divisions of the trachea
- Right main bronchus is wider and deviates less from the axis of the trachea (the left main bronchus has a tighter turn over the heart), which is why foreign bodies will tend to the right side
- The two main bronchi divide into a total of 5 lobar bronchi, which in turn divide into a total of 18 segmental bronchi
- Right main bronchi is ~2cm long
- Left main bronchi is ~5cm long
- Cross-sectional area of the respiratory tract is lowest at the third division
- These bronchi will collapse when intrathoracic pressure exceeds intraluminal pressure by ~5cmH2O.
- Segmental bronchi travel with branches of the pulmonary artery and lymphatics
These are the bronchi that demonstrate peribronchial cuffing and perihilar haze in early pulmonary oedema. - Flow is typically transitional in the smaller bronchi and bronchioles
- Bronchioles
- Embedded in the lung parenchyma
- Do not have cartilage in their walls to maintain patency - are held open by lung volume
- Resistance to flow tends to be negligible due to large cross sectional area, unless there is spasm of helical muscle bands in bronchial wall
- Terminal bronchioles
- Flow may become laminar in the smallest bronchioles as flow decreases
- Trachea
- Flow in the conducting zone during inspiration is fast and turbulent
- No gas exchange occurs in the conducting zone
The volume of the conducting zone therefore contributes to anatomic dead space. - Blood supply to the conducting zone is via the bronchial circulation
- Mucous is secreted by goblet cells in the bronchial walls to trap inhaled particles
- Cilia in the bronchial walls move rhythmically to drive the mucociliary elevator, driving mucous up to the epiglottis, where it is then swallowed or expectorated
Respiratory Zone
The remaining 7 divisions make up the respiratory zone. This region:
- Makes up the majority of lung volume
All non-anatomical dead space volume is in the respiratory zone, and is ~30ml.kg-1 (FRC) at rest - Blood supply is via the pulmonary circulation
- Gas flow in the terminal respiratory zone is slow due to the exponential increase in cross-sectional area with each airway division
- Diffusion is the predominant mechanism of gas movement
Alveolus
The alveolus is optimised for gas exchange:
- Spherical shape maximises surface area to volume ratio
- Total surface area of lung alveoli is 50-100m2
- Alveolar walls are extremely thin (0.2-0.3μm)
Consequently, they are fragile and can be damaged by increases in capillary pressure - Alveolar walls contain a dense mesh of capillaries 7 to 10μm thick, which is just large enough for an erythrocyte to pass through
The alveolar-capillary barrier consists of three layers:- Type I pneumocytes
- Extracellular matrix
- Pulmonary capillary endothelium
Alveoli are composed of three types of cells:
- Type I pneumocytes
Thin-walled epithelial cells optimised for gas exchange.- Form ~90% of the alveolar surface area
- Type II pneumocytes
Specialised secretory cells.- Secrete surfactant
Alveoli are inherently unstable, and surface tension of alveolar fluid favours collapse of the alveoli. Surfactant reduces surface tension, allowing the alveoli to expand. - Form ~10% of alveolar surface area
- Secrete surfactant
- Alveolar macrophages
Alveoli have no cilia - inhaled particles are phagocytosed by alveolar macrophages in alveolar septa and lung interstitium.
References
- Lumb A. Nunn's Applied Respiratory Physiology. 7th Edition. Elsevier. 2010.
- West J. Respiratory Physiology: The Essentials. 9th Edition. Lippincott Williams and Wilkins. 2011.
- Chambers D, Huang C, Matthews G. Basic Physiology for Anaesthetists. Cambridge University Press. 2015.